After my daughter’s OmniPod insulin pump pod emitted a high pitched continuous alarm during a midterm, she decided to switch back to the Tslim insulin pump. The alarm interrupted everyone taking the exam, and she had to get up and leave the room while the pod still alarmed. She went to the nurse’s office and changed her pod (all by herself!) and had to make up the rest of her midterm exam on another day after school.
Having no tubing was a real perk to the Omnipod, but it is a relief to not have to carry the PDM device everywhere to administer the insulin (or to have to find it when you need to give insulin). It is also a relief to not have to worry about what you will be doing in three days’ time when it’s time to change the infusion set. (Will the time-to-change-the-pod reminder alarm go off during class? During band practice? During the night while sleeping?) Recently we went away for three days and she had to change the pod while traveling on day 2. It would have been nice to have had the option to wait until we got home. We definitely won’t miss the forced pod changes exactly every three days.
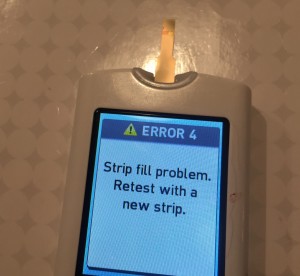
The other irksome thing about the OmniPod is that after you change the pod, two hours later the pod alarms to tell you to check your blood sugar. This alarm is incredible patronizing and can occur during the night or at any other inconvenient time. Since my daughter is using the Dexcom G5 CGMS, the alarm seems obsolete as well, since she can just look at the Dexcom anytime, and it will alarm for highs and lows. Of course, it’s just another way diabetes disrupts your life, and in this case it’s a manmade interference. Even with her pump settings on vibrate, the alarm is still disruptive. It makes you think there’s a problem, such as a low insulin cartridge or a low battery, filling you with dread for no good reason. Also the PDM as a glucometer worked more slowly than her previous meter (which was the Verio), so it was another way diabetes steals moments of your life.
The Tslim pump has simplified her day at school as well. On the OmniPod, she would have to remember to take her PDM device out of her book bag and put it in her lunch bag. And if she forgot it, she would have to go back to her locker to get it. Then she would have to take it out of her lunch bag to bolus the insulin to cover for her lunch. Now with the Tslim, she can use the quick bolus without taking the insulin pump out of her belt.
On the other hand, when I check her blood sugar during the night, now I need to find the pump under the covers to correct her blood sugar if it’s high, since the Tslim doesn’t have a remote device. I also risk waking her up while I do this which wasn’t an issue with the OmniPod. And if she needs a small correction bolus, I have to decide whether it’s worth the risk of waking her up during the night.
Now that it is summertime, my daughter has switched back to the OmniPod! Now she doesn’t have to be disconnected from her insulin pump for long periods of time during swim team practices and swim meets, since the Tslim is not waterproof. It is now nice to be able to adjust basal rates from the remote device and to do temp basal rates from the PDM which is also useful for swim practices and meets. At least during the summer, she doesn’t have to worry about the alarms going off during class or exams, and I anticipate she will switch back to the Tslim before school starts.
It just goes to show you that not only do different insulin pumps meet different people’s needs (my other daughter remains on the Animas pump, for example), but also that different pumps can meet one person’s needs at different times. It also reflects that there still isn’t one pump that addresses all the needs.
And having a backup pump in case of pump failure is also a bonus.
Disclosure: I have no financial interest in any diabetes company and have received no money or gifts to write this blog post. Please keep in mind that these are just my juicy experiences and opinions, which will vary from someone else’s.